
Recurrent abdominal pain attributed to pancreatitis
An 18-year-old woman with a complex past medical history presented with 2 days of vomiting and lower abdominal pain.
Case adapted with permission from Corden MH, Frediani J, Xu F, et al. An 18-Year-Old With Acute-on-Chronic Abdominal Pain. Pediatrics. 2018;141(5):e20171332

Patient reported
- 8 out of 10 crampy, lower quadrant, non-radiating abdominal pain
- Several days of reduced oral intake because of nausea
- Worsening of her chronic constipation, with her last bowel movement 2 days before admission
- 40-lb unintentional weight loss over the past 4 months
No upper respiratory symptoms, rash, fevers, or chills. No recent travel history or trauma. She denied alcohol or illicit drug use.
Past medical history – 5 months before admission
- Chronic constipation
- Hospitalized on 4 separate occasions for abdominal pain, nausea, and vomiting
- Episodes were often accompanied by
- Hypertension
- Back pain
- Intermittent paresthesias of the lips, abdomen, and legs
Workup – 5 months before admission
| Test | Result |
| CT scan | Negative for pancreatic inflammation, pseudocysts, or ascites |
| Abdominal ultrasound | Demonstrated either biliary sludge or a small gallstone, and she underwent laparoscopic cholecystectomy – symptoms persisted |
| MRI and MRCP | Intrahepatic biliary ductal dilatation and a heterogeneous pancreas without focal lesions or pseudocysts |
| Endoscopic retrograde cholangiopancreatography | Stenosis of the pancreatic sphincter |
CT = computed tomography; MRI = magnetic resonance imaging; MRCP = magnetic resonance cholangiopancreatography
A stent was placed, resulting in symptom improvement and a decreased lipase. Despite these interventions, her symptoms recurred.
Initial physical exam upon admission
- Tachycardia (110–120 seconds)
- Hypertension (130s over 80s)
- Diffuse abdominal tenderness to light palpation
- Initial exam was otherwise unremarkable
Initial laboratory tests upon admission
- Elevated liver enzymes
- Aspartate aminotransferase 68 U/L
- Alanine aminotransferase 80 U/L
- Normal lipase which increased over the next few days 1707 U/L
One element of her history that could not be explained by pancreatitis was her initial complaint of paresthesias of the lips and legs.
Hospital day 5
- Began staring blankly into space and was minimally responsive to verbal or tactile stimulation
- Developed bilateral weakness in wrist flexion and reduced grip strength
- Hyponatremic (sodium 114 mEq/L)
After slow correction with hypertonic saline, her mental status improved, but her distal muscle weakness persisted. Neurology was consulted, but the patient’s findings did not correspond with a particular pathology. The neurologists recommended outpatient electromyography.

Clue – Dark or red-colored urine
On further history, her mother noted that the patient’s urine had been red-colored during her hospitalization. Her urine test results were negative for blood or infection.
These new findings prompted her team to consider an acute porphyria as a unifying diagnosis.
Urine porphobilinogen (PBG) was elevated at 116.8 mg/L, confirming suspicion. Given the limited experience with the porphyrias at this institution, hematology was consulted.
Symptoms plus elevated PBG: Is it an acute hepatic porphyria?
Patient’s symptoms of recurrent abdominal pain, intractable nausea, hypertension, hyponatremia, and muscle weakness in the setting of a significantly elevated urine PBG were consistent with the diagnosis of an acute hepatic porphyria.
Hematology recommended obtaining a urine δ-aminolevulinic acid (ALA) and quantitative urine porphyrins, fecal porphyrin levels, plasma porphyrins, and erythrocyte PBG deaminase levels.
Differentiating the subtype of acute hepatic porphyrias
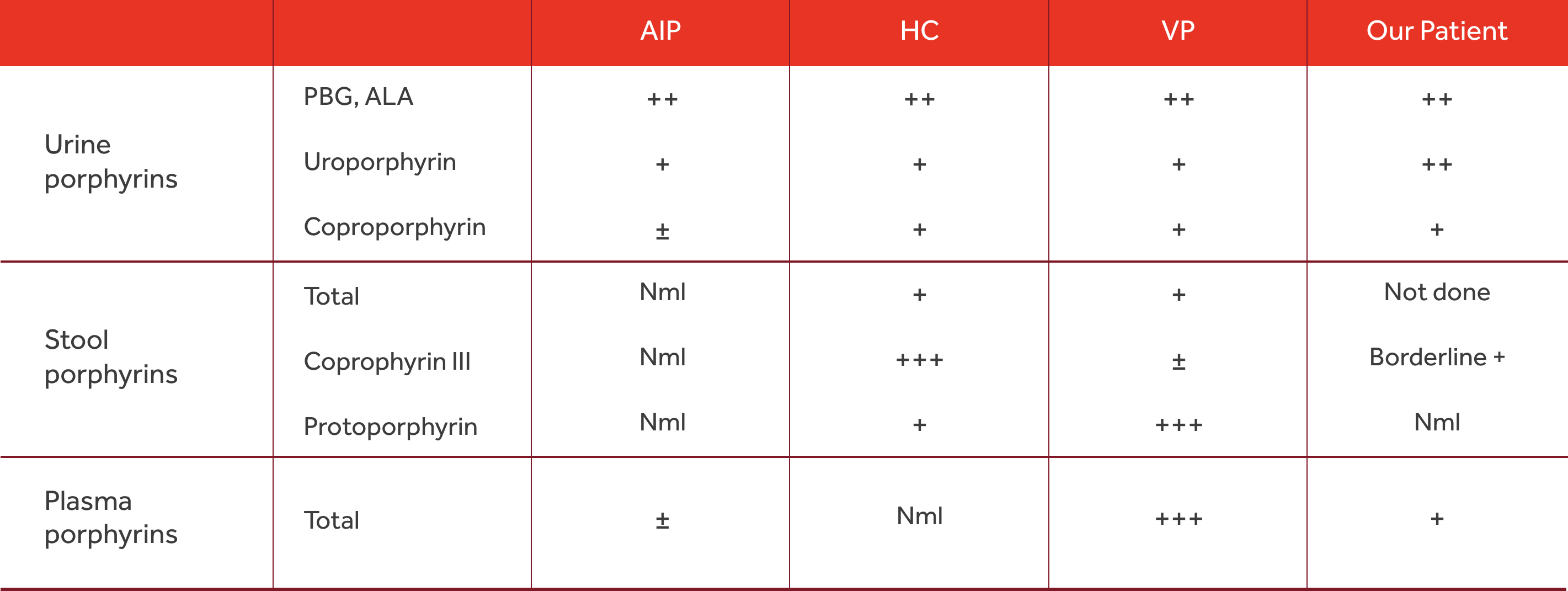
HC = hereditary coprophyria; Nml, normal; VP = variegate porphyria
Final diagnosis – Acute Intermittent Porphyria (AIP)
After being hospitalized for more than 3 of the previous 5 months, the patient’s laboratory evaluation helped confirm her underlying diagnosis, AIP.
Clinical symptoms of AIP (symptoms experienced by our patient are in red)
| Category | Symptom |
| Increased sympathetic activity |
Tachycardia Hypertension Palpitations and/or arrhythmias Sweating Urinary retention
|
| Visceral symptoms |
Abdominal pain (steady and poorly localized) Constipation Nausea and/or vomiting
|
| Neurologic symptoms |
Headache Muscle weakness Neuropathic pain Tremors Seizure Sensory loss
|
| Psychiatric symptoms |
Anxiety Depression Disorientation and/or hallucinations Insomnia Paranoia Restlessness
|
Conclusion
AIP can present with a wide variety of symptoms and may mimic more common diseases. A diagnosis of acute porphyria can be considered when the traditional historical elements, physical examination findings, and diagnostic parameters do not follow the typical progression of the working diagnosis.
Delay in arriving at the diagnosis of AIP is not uncommon and has been associated with an increase in mortality.