An Unusual Case of Abdominal Pain and Hyponatremia in a 16-Year-Old Girl with Disordered Eating
A previously healthy, 16-year-old girl presented to the emergency department (ED) with 1 week of abdominal pain and constipation.
Adapted with permission from Hunter G, et al. Pediatrics. 2018 Jan;141(1).

- Symptoms began several days after she decreased caloric intake to lose weight
- Drinking 48 to 60 oz of water per day for several days before admission to ameliorate constipation
- Admitted to drinking alcohol the night before pain began
- No known history of diarrhea, rectal bleeding, melena, or dysuria
- Last menstrual period ended 3 days before presentation
- Visited several other EDs before admission and had been sent home with instructions to manage constipation at home
- On arrival to ED, she describes severe diffuse abdominal pain
- On physical examination, she appears anxious and in significant pain
- Vital signs:
- Temperature = 36.7°C
- HR = 81 bpm
- RR = 20 bpm
- BP = 137/75
- Abdomen is tender to palpation throughout but soft with no rebound tenderness or peritoneal signs
- Remainder of examination yields normal results

- Consider the following:
- Intestinal obstruction
- Peptic ulcer disease
- Diabetic ketoacidosis
- Because she is an adolescent girl, it is also important to consider ectopic pregnancy and obtain a urine pregnancy test, even if the adolescent denies previous sexual activity
- Less common causes of acute abdominal pain in adolescents include pancreatitis, acute cholecystitis, intra-abdominal abscess, abdominal migraine, poisoning, and acute porphyrias
- Standard workup for patients with abdominal pain consists of:
- Complete blood cell count
- Electrolytes
- Renal function tests
- Liver function tests
- Lipase
- Most patients should also get a urinalysis, and girls of reproductive age should receive a urine pregnancy test
- Depending on the history and physical examination, abdominal imaging (including radiograph, ultrasound, or computed tomographic scan) may be needed
- Pelvic examination should be considered for all female patients depending on the location and quality of their abdominal pain
Test Results
- Complete blood count, liver function tests, and lipase were all within normal limits
- She was found to have hyponatremia with a sodium level of 122, but her serum urea nitrogen level, creatinine level, and other electrolyte levels were normal
- Initial urinalysis showed a specific gravity of 1.008 and was otherwise unremarkable
- Urine pregnancy test result was negative
- Abdominal radiograph showed nonspecific gaseous distension of the colon and moderate stool
- Admitted to the general pediatrics service for bowel cleanout and pain control
- Constipation and drinking a significant amount of water may be the cause of the patient’s abdominal pain and hyponatremia respectively, but it is important to consider other diagnoses
- She was not symptomatic from the hyponatremia; therefore, it could be because of a more chronic etiology
Resolution of hyponatremia and constipation
- Hyponatremia was corrected
- Once hyponatremia resolved, she successfully underwent a bowel cleanout
- Despite adequate treatment of her constipation, including a follow-up radiograph showing resolution of stool burden, the patient continues to have significant abdominal pain
- The home, education, activities, drugs, sex, suicide, and safety assessment revealed several stressors, including a recent suicide in the family and a history of disordered eating and anxiety
- Although it is rare, her constellation of symptoms (hyponatremia, abdominal pain, and psychiatric symptoms in an adolescent girl) may be caused by AIP
- Quantitative urine porphobilinogen (PBG) was sent and came back elevated at 284.6 mmol/L (normal 0–8 mmol/L), which is suggestive of AIP
- Pediatric hematology was consulted – After further questioning, the family history was notable for psychiatric illness in several other members of the family
- The patient stated that she had always had “dark urine”
Conclusion
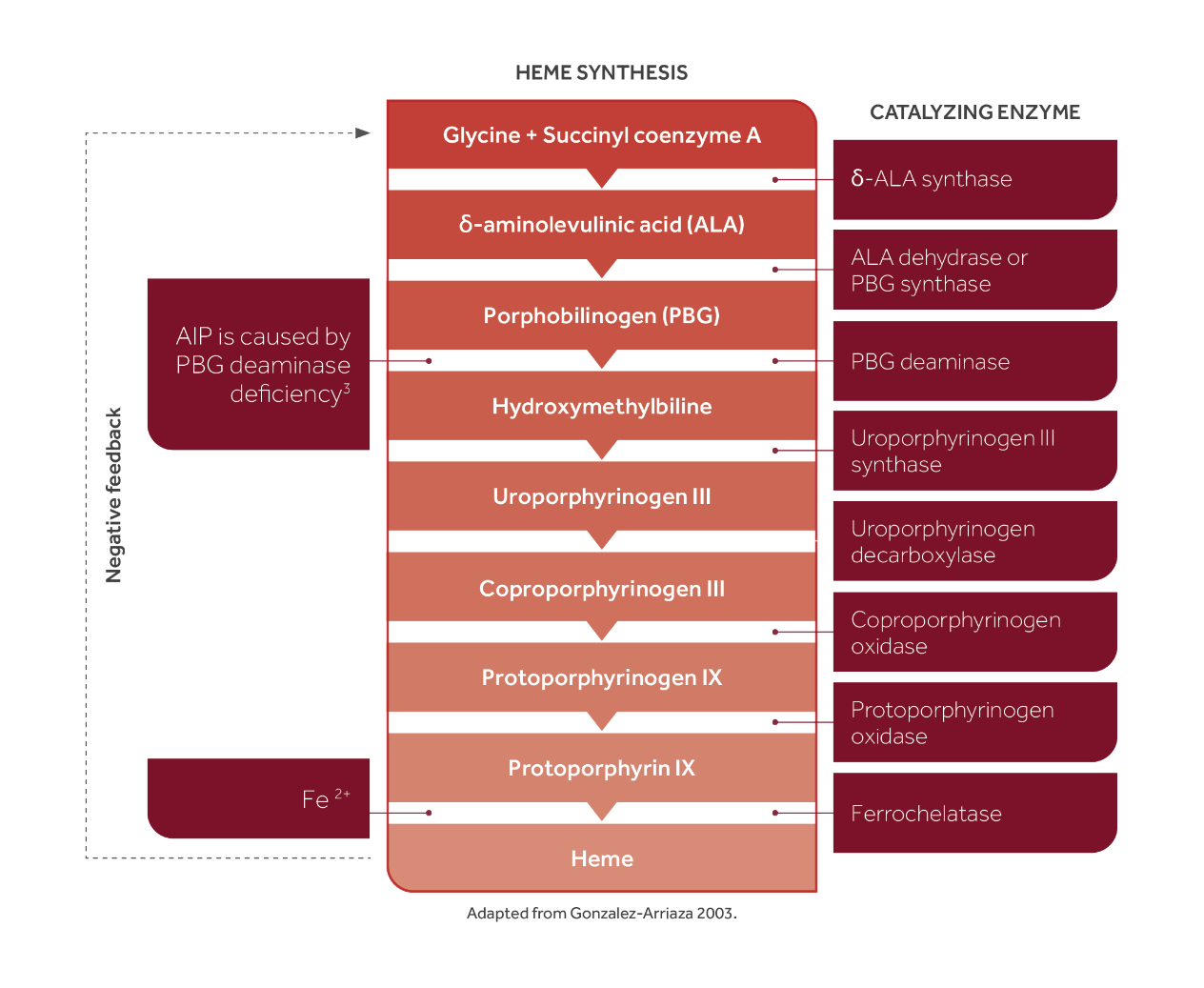
- AIP is a rare disorder caused by a mutation in one of the enzymes in the heme pathway, which leads to a buildup of porphyrin precursors
- One of the most common triggers for AIP is starvation, and the patient does have a history of disordered eating with a recent decrease in her caloric intake
- Although an elevated urine porphobilinogen test, along with her constellation of symptoms, is highly suggestive of AIP, genetic testing looking for the most common enzyme mutations in the heme pathway should confirm the diagnosis
The potential harms of missing the diagnosis can be severe and costly. This case highlights the importance of considering “zebras” when the signs and symptoms of a clinical case do not match the more common diagnoses.
Abbreviations:
AIP = acute intermittent porphyria
BPM = beats per minute
BPM = breaths per minute
BP = blood pressure
HMBS = hydroxymethylbilane synthase
HR = heart rate
RR = respiratory rate
Want to know more?